March 15, 2022
Updated: September 28, 2022
By: Kenneth E. Thorpe. Ph.D.
The Food and Drug Administration’s accelerated approval pathway was created to hasten access to safe and effective new therapies for people living with serious or life-threatening conditions where treatment options are limited or non-existent. Without this pathway, people suffering from certain cancers, genetic conditions, or HIV/AIDS would face avoidable disease progression, preventable disability, and premature death.
Today, efforts are underway that would undermine the pathway, particularly within the Medicaid program, putting some of our most vulnerable residents at risk. Spending concerns are among the primary reasons cited by states seeking to limit access to these medicines. With this in mind, last year, we analyzed national Medicaid drug spending data from 2007 through 2018 to determine if accelerated approval drugs were a driver of spending within the program. Using data from the National Health Accounts and State Medicaid prescription drug data tabulated by the Centers for Medicare and Medicaid Services (CMS) we found that Medicaid spending on accelerated approval drugs remained steady at 0.6% to 0.8% of total spending year over year. These numbers hold true, even after the passage of the Food and Drug Safety and Innovation Act in 2012, which encouraged accelerated approval use for rare conditions in addition to oncology and HIV/AIDS and after the 2010 Affordable Care Act expanded Medicaid access.
In a commentary published in the American Journal of Managed Care, we concluded that “Medicaid programs seeking ways to meaningfully mitigate budgetary impacts from rising health care costs will not find success in restricting or eliminating coverage of accelerated approval drugs… Accelerated approval drugs account for less than 1% of overall Medicaid spending while often representing the only treatment options available for beneficiaries.”
Given ongoing criticisms by state Medicaid programs about drugs approved through the accelerated approval pathway and, specifically, efforts by individual state Medicaid programs to waive their federal obligation to cover these drugs, we embarked on a state-based complement to our original analysis in addition to updating the national data through 2020. Since most drugs approved using accelerated approval convert to traditional FDA approval once confirmatory clinical trials are completed, we also calculated spending data accounting for those conversions to traditional approval.
These updated findings show that, based on CMS data for each state, the average spending on accelerated approval drugs in relation to state’s total Medicaid spending was 0.21%. Overall, spending on accelerated approval drugs as a share of total Medicaid spending for a state ranged from 0.03% to 0.72%, despite wide variations in state program size, demographics, and eligibility criteria.
These findings are particularly important considering that, when requesting access restrictions for accelerated approval drugs through so-called 1115 waivers, states have claimed that accelerated approval drugs have an outsized impact on their state budgets. To date, three states – Tennessee, Massachusetts, and Oregon – have requested CMS waive Medicaid drug coverage requirements for accelerated approval therapies.
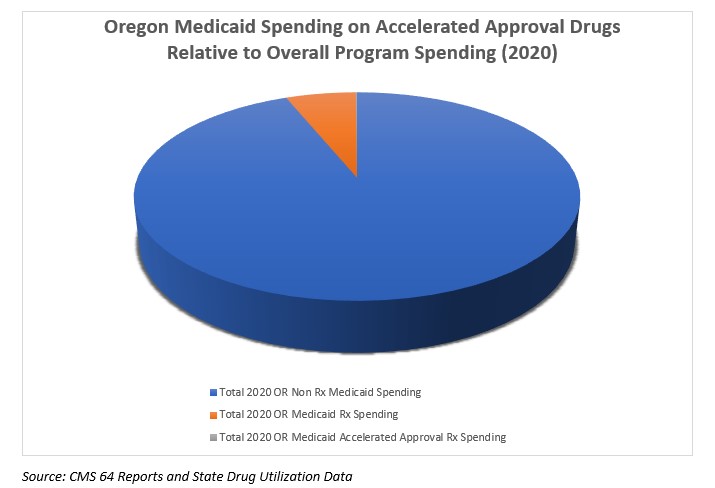
The most recent waiver request – one that’s currently pending with CMS – is from Oregon. In making their budget impact argument, the Oregon Health Authority conflates accelerated approval drugs and the much broader category of “specialty medicines” in arguing for authority to deny access over time. They state: "New drugs approved under the FDA’s accelerated approval pathway tend to be specialty medications that represent a significant portion of pharmacy expenditures." Our data shows that accelerated approval drugs, in fact, represent a miniscule portion of pharmacy expenditure.
Our initial analysis finds that, in 2020, accelerated approval drugs accounted for only 0.11% of total Medicaid spending in Oregon and, between 2015 and 2020, the category represented just 0.2% of total Medicaid spending growth, relative to the 31% growth in total Medicaid spending in that state during that same span.
Clearly, accelerated approval drug costs are not driving Oregon’s Medicaid spending. Asserting otherwise is a red herring in the state’s overall position that the Oregon Health Authority is better equipped to use its own review process to determine if an accelerated approval drug is safe and effective and should be covered. The proposal, if approved, sets a dangerous precedent for patients in Oregon and elsewhere. Such an approach not only usurps FDA’s authority as the sole determiner of safety and efficacy, but also undermines patient protections inherent in the Medicaid program and doesn’t alleviate Medicaid spending concerns.
As CMS weighs Oregon’s application, it is critical that stakeholders make their voices heard on this issue. The Partnership to Fight Chronic Disease stands by our original opposition to Oregon’s proposal and urges CMS to reject the care limitations included within the proposed waiver and instead guide OHA to work to preserve access protections for Medicaid beneficiaries afforded under federal law. You can comment on Oregon’s proposal HERE.
Note: This blog was updated to reflect completion of Medicaid spending analysis and consideration of transitions of drugs from accelerated to traditional FDA approval status. Spending on accelerated approval drugs does not account for any drug rebates. As such, actual spending and spending contributions will be lower than those estimated here.
On September 28, 2022, CMS approved Oregon's 1115 Demostration Waiver without the provision to exclude coverage for prescription drugs approved using the accelerated approval pathway. The full Demostration Approval can be found HERE, and the exclusion referenced below, noting the state's removal of the request from the application.
"The most frequent themes among comments opposing the demonstration were concerns about the Prioritized List and the proposed changes to prescription drug coverage. Concerns about the Prioritized List included objections to the use of the Quality Adjusted Life Years measure as evidence for certain treatments, claims that the list does not align with the goals of the EPSDT benefit, and criticism for the lack of a legitimate appeals process for the services not covered by the Prioritized List. Commenters argued that this request would hamper progress toward health equity and that continued approval of the Prioritized List would limit access to essential health care services for Medicaid beneficiaries, therefore widening disparities. CMS acknowledges these concerns about the Prioritized List, and, as described above, the state is planning to phase out the waivers of amount, duration, and scope and the waiver of the requirement to provide EPSDT benefits. Commenters also raised concerns about how the state’s requested prescription drug coverage flexibilities could restrict beneficiary access to critical medicines. The state removed this request from their application."
For more on accelerated approval, please visit www.fightchronicdisease.org/resources/acceleratedapproval for issue background, economic analyses, an American Journal of Managed Care commentary, infographics, opinion editorials and podcasts.

